One Platform for All Your Ultrasound Training Needs
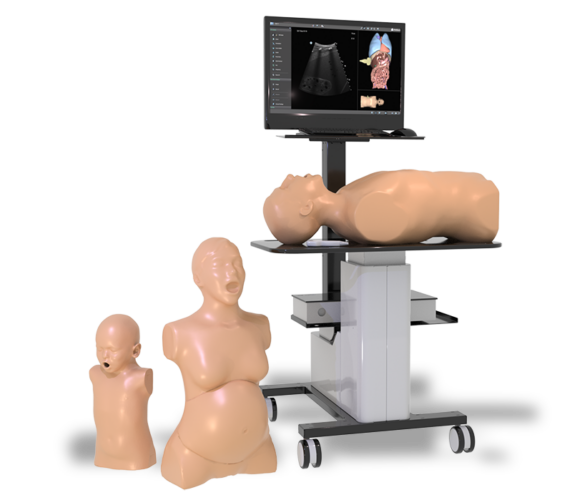
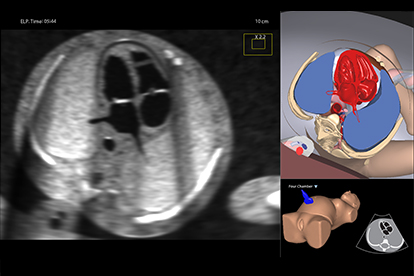
Simbionix Ultrasound Mentor is the answer to the growing need for ultrasound training among multiple medical specialties. This modular simulation platform enables easy manikin rotation (male, female, pediatric and interventional), and offers diverse applications for a range of specialties such as OB/GYN, Point-of-care Ultrasound (POCUS) and Echocardiography.
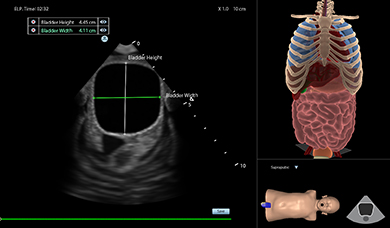
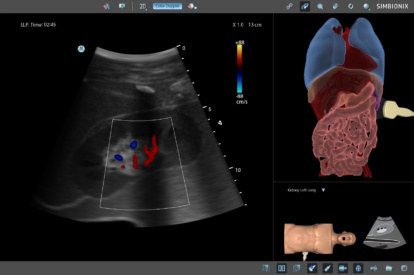
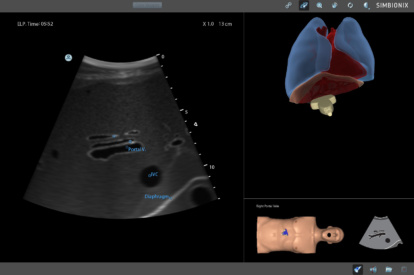
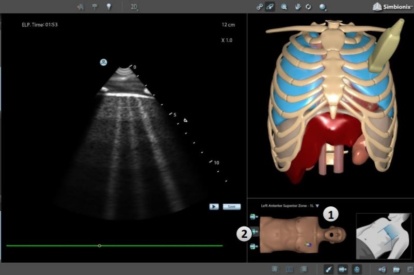
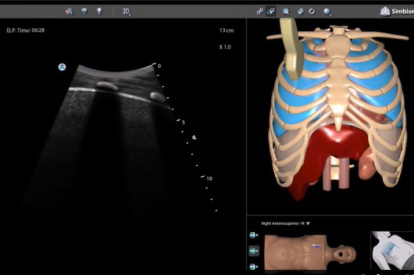
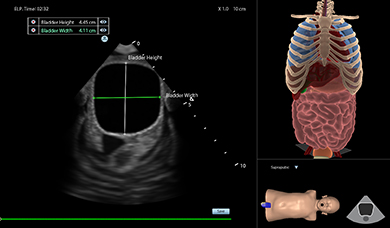
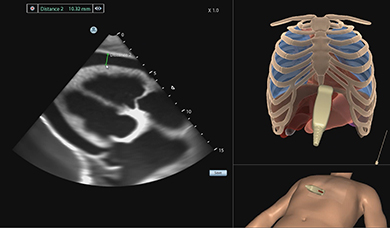
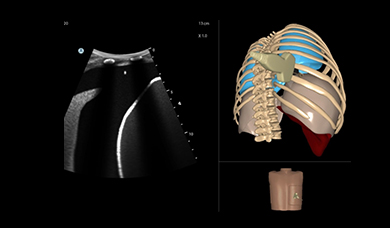
Ultrasound Mentor accelerates the development of basic to advanced technical and cognitive skills, by providing not only the probe manipulation training, but also a didactic environment enabling structured, self-guided learning including step-by-step instructions and educational aids such as 3D anatomical map and probe positioning assistant, all backed up with our progress monitoring tool MentorLearn.
How Is Ultrasound Mentor Used in Medical Schools?
See how Dr. Charles DeMesa, Pain Medicine Program Director at UC Davis uses it.
Features and Benefits
- A modular platform with easy manikin rotation
- Quick probe switch between TTE/TEE and TAS/TVS approaches
- A selection of virtual and real patient cases, with the ability to modify case severity
- Step-by-step tasks provide a self-learning opportunity for sonography skills and scanning protocols
- Advanced diagnostic tools, including Color Doppler, CW, PW, M-mode, and measurements
- Ongoing metrics capturing for accuracy and efficacy measurements including image analysis
- MyCase software enables the creation of a custom case for every need, based on a real scan
- An immersive learning experience with VR goggles and a designated probe add-on
Modules
EFAST and RUSH MODULE
Abdominal Module
Advanced Abdominal Module
Covid-19 Module
Lung Module
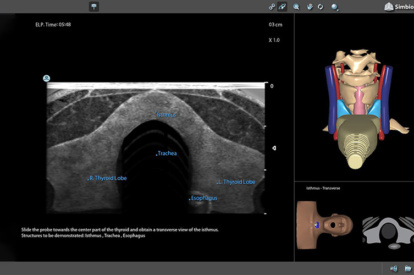
Neck Module
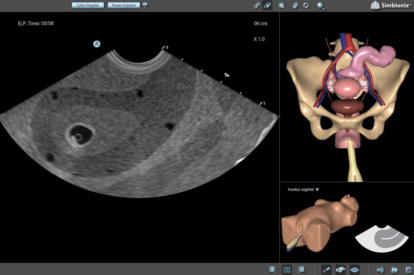
Basic GYN Module
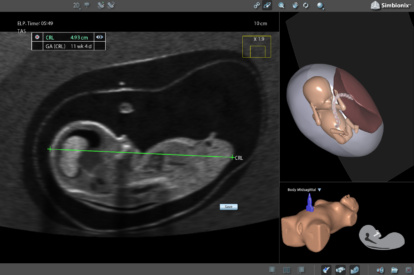
OB 1st Trimester Module
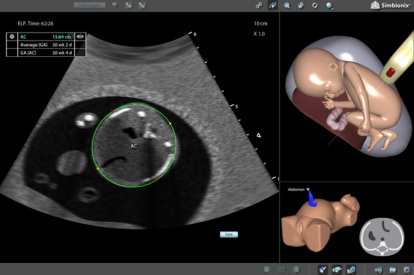
OB 2nd Trimester Module
Fetal Echo Module

Fetal Neurosonography Module
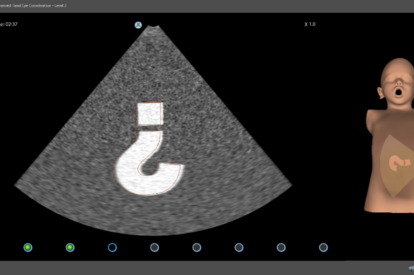
Pediatric Basic Skills Module
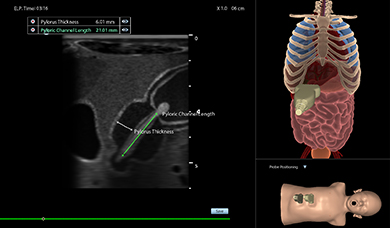
Pediatric Abdominal Module
Pediatric eFast Module
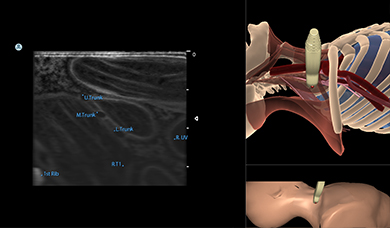
Brachial Plexus Nerve Block Module
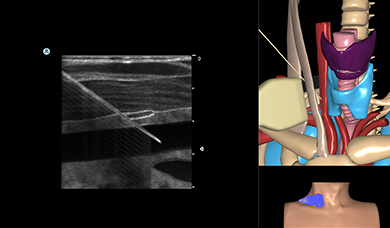
Central Line Ultrasound Module
Pericardiocentesis Ultrasound Module
Thoracentesis Module
Sonography Basic Skills Module
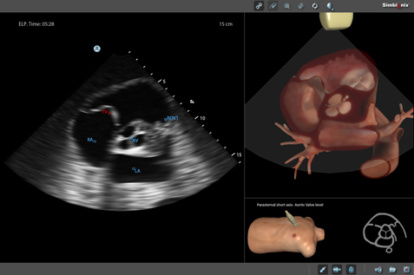
Bedside Echocardiography Module
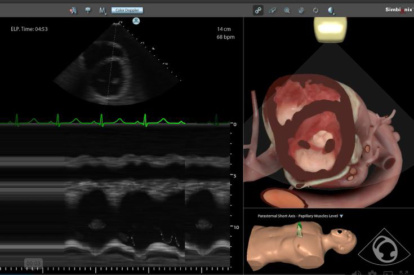
Advanced Echo Module
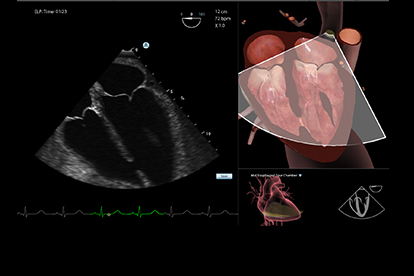
TEE Module
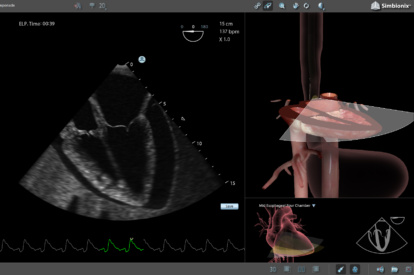
TEE Emergency Module
Testimonials
“The Ultrasound Mentor Platform has been an invaluable learning resource and tool for our medical and physician assistant students, residents, and faculty. Our learners are more fully engaged and immersed…
Bill Boyer, MD
Associate Dean – Graduate Medical Education & Faculty Development at the Florida State University College of Medicine
“The Surgical Science Transesophageal Echocardiography (TEE) Express simulator has proven invaluable in enhancing emergency physicians' skills by providing an easily set-up platform for repeated practice…
Dr. Edmund Hsu
Director of Ultrasound in Medical Education at University of California, Irvine
“The simulator has allowed our residents, fellows and sonographer students to systematically review fetal anatomy. The fetal movement during the exam replicates real life scanning in a way that dramatically…
Terry C Harper, MD
University of Colorado Anschutz Medical Campus
“We have used the Ultrasound Mentor extensively, and I recommend it very strongly to train fellows in cardiology and cardiac anesthesiology to improve their TEE skills and practice performing comprehensive…
Dr. Jyothy Puthumana
Feinberg School of Medicine
"Working with the Ultrasound Mentor helps shorten our students' learning curve, both in terms of their scanning capabilities and improved clinical reasoning. Learning new scanning protocols in a scaled,…
Professor Sanja Kupesic Plavsic
L. Foster School of Medicine Texas Tech University
Validation Studies
We developed a test for the assessment of clinical competences in basic thoracic ultrasound with solid validity evidence, and a pass/fail standard with no false positives or false negatives.
Simulation-based teaching of TEE showed a significant improvement in the knowledge, skills, and self-assessment of proficiency of cardiology fellows, as well as a reduction in the amount of time needed to complete the examination. These results should encourage further investigation of clinical performance and patient benefits of TEE simulation training.
Learn More
Download the Ultrasound Mentor Brochure
Learn more about the Ultrasound Mentor simulator.

Contact Us
Do you want to know more about the Ultrasound Mentor?