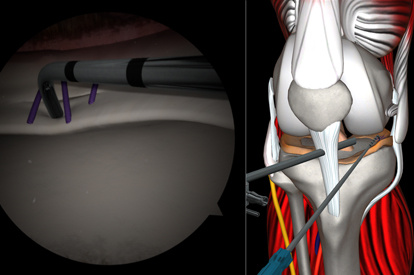
A Highly Effective and Validated Simulator for Core Arthroscopy Skills Acquisition

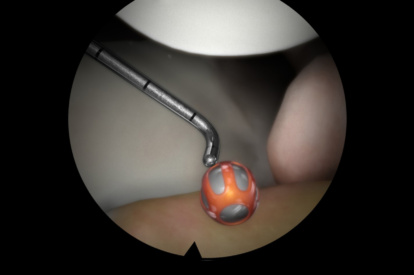
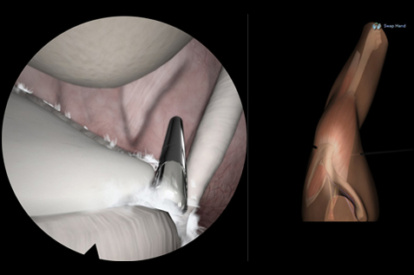
ARTHRO Mentor is an effective tool for arthroscopic surgery skills acquisition. With over 15 years of validation studies, it offers a line of simulated procedures, covering the 3 major joints (shoulder, knee, and hip) combining physical anatomical models with 3D images and dynamic haptic sensation, to allow users to learn key aspects of the procedures while providing tissue sensation.
Enjoy a safe and controlled environment for trainees to gain hands-on experience, with comprehensive and structured programs ideal for both novice and advanced learners and ready-to-use courses for independent training. With detailed feedback on the trainee’s performance, the ARTHRO Mentor simulator is a must-have tool for any arthroscopic surgical training program.
See How Dr. Mathew Sardelli Uses The ARTHRO Mentor To Prepare Residents
Features and Benefits
- Reduces training time and improves the learning curve
- A comprehensive didactic environment
- Self-learning structured curriculum in collaboration with KOLs
- Competence assessment based on performance metrics
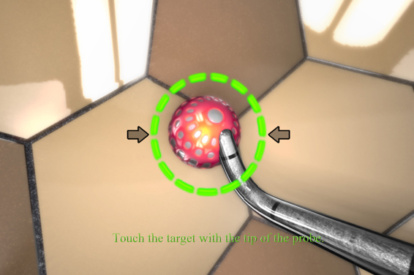
- Adaptive tactile sensation on drilling, suturing, and shaving
- A library of modules with 80+ tasks, cases, and didactics
- Interchangeable knee, shoulder and hip models
Testimonials
“I want to go on record as recommending the ARTHRO Mentor virtual reality simulator for shoulder arthroscopy for any training institution that plans to maximize the opportunity to train surgeons in…
Stephen J. Snyder, MD
Southern California Orthopedic Institute
“The ARTHRO Mentor is the wave of the future. It allows us to give our residents a tool that can train them in those types of arthroscopic skills that they really can’t get other than actually using…
Sherwin Ho, MD
Associate Professor and Director, Sports Medicine Fellowship, University of Chicago
“I think that arthroscopy really lends itself to simulation and with the Surgical Science simulator there’s tactile feedback that really gives the resident or the trainee a good sense of what it’s like…
Bradley Dunlap, MD
Clinical Assistant Professor, NorthShore Medical Group, Chicago
“We found that residents beginning the five year residency program didn’t have the necessary skills to succeed in the operating room as it pertained to arthroscopy. They didn’t know how to hold the…
Mathew Sardelli, MD
Orthopedic Surgeon specializing in Sports Medicine, McLaren Flint, Michigan
“The ARTHRO Mentor virtual reality arthroscopic simulator is the most advanced virtual reality simulator system for teaching and training arthroscopy surgery”.
Ofer Levy
BESS (British Elblow and Shoulder Society) Education Committee
“It certainly has proven to be the most realistic simulator I have found on the market thus far”.
Lennard Funk, MD
Consultant Shoulder & Upper Limb Surgeon, Manchester Sports Medicine Clinic and Wrightington Hospital, Manchester, UK
Validation Studies
This comparative cross-sectional study contrasts the automated performance reports for novice and expert orthopedic surgeons after executing surgical tasks on the ARTHRO Mentor virtual reality simulator. Setting Surgical simulation center at the University of Chile Clinical Hospital, Santiago, Chile. ARTHRO Mentor simulator for knee arthroscopy showed good construct validity, with performance metrics accurately discriminating between expert and novice users.
The results of this study demonstrate learning curves for a hip arthroscopy simulator, with significant improvements seen after three sessions. All performance metrics were found to improved, demonstrating sufcient visuo-haptic consistency within the virtual environment, enabling individuals to develop basic arthroscopic skills.
Learn More
Download the ARTHRO Mentor Brochure
Learn more about the ARTHRO Mentor simulator.

Contact Us
Do you want to know more about the ARTHRO Mentor?